Page 4 - 2022 01 Benefits Guide Murata Flipbook Final 6.14.22
P. 4
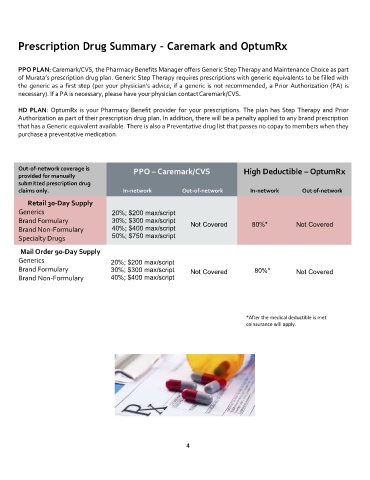
Prescription Drug Summary – Caremark and OptumRx
PPO PLAN: Caremark/CVS, the Pharmacy Benefits Manager offers Generic Step Therapy and Maintenance Choice as part
of Murata’s prescription drug plan. Generic Step Therapy requires prescriptions with generic equivalents to be filled with
the generic as a first step (per your physician’s advice, if a generic is not recommended, a Prior Authorization (PA) is
necessary). If a PA is necessary, please have your physician contactCaremark/CVS.
HD PLAN: OptumRx is your Pharmacy Benefit provider for your prescriptions. The plan has Step Therapy and Prior
Authorization as part of their prescription drug plan. In addition, there will be a penalty applied to any brand prescription
that has a Generic equivalent available. There is also a Preventative drug list that passes no copay to members when they
purchase a preventative medication.
Out-of-network coverage is PPO – Caremark/CVS High Deductible – OptumRx
provided for manually
submitted prescription drug
claims only. In-network Out-of-network In-network Out -of-network
Retail 30-Day Supply
Generics 20%; $200 max/script
Brand Formulary 30%; $300 max/script Not Covered 80%* Not Covered
Brand Non-Formulary 40%; $400 max/script
Specialty Drugs 50%; $750 max/script
Mail Order 90-Day Supply
Generics 20%; $200 max/script
Brand Formulary 30%; $300 max/script Not Covered 80%* Not Covered
Brand Non-Formulary 40%; $400 max/script
*After the medical deductible is met
coinsurance will apply.
4