Page 194 - pharma 1 theoretical updated MNU_Neat
P. 194
Clinical pharmacy 2024/2025 Level 3 Pharm D Pharmacology 1 (PO 502)
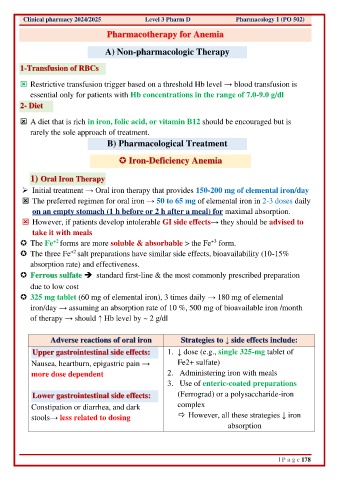
Pharmacotherapy for Anemia
A) Non-pharmacologic Therapy
1-Transfusion of RBCs
Restrictive transfusion trigger based on a threshold Hb level → blood transfusion is
essential only for patients with Hb concentrations in the range of 7.0-9.0 g/dl
2- Diet
A diet that is rich in iron, folic acid, or vitamin B12 should be encouraged but is
rarely the sole approach of treatment.
B) Pharmacological Treatment
Iron-Deficiency Anemia
1) Oral Iron Therapy
➢ Initial treatment → Oral iron therapy that provides 150-200 mg of elemental iron/day
The preferred regimen for oral iron → 50 to 65 mg of elemental iron in 2-3 doses daily
on an empty stomach (1 h before or 2 h after a meal) for maximal absorption.
However, if patients develop intolerable GI side effects→ they should be advised to
take it with meals
+3
+2
The Fe forms are more soluble & absorbable > the Fe form.
+2
The three Fe salt preparations have similar side effects, bioavailability (10-15%
absorption rate) and effectiveness.
Ferrous sulfate ➔ standard first-line & the most commonly prescribed preparation
due to low cost
325 mg tablet (60 mg of elemental iron), 3 times daily → 180 mg of elemental
iron/day → assuming an absorption rate of 10 %, 500 mg of bioavailable iron /month
of therapy → should ↑ Hb level by ~ 2 g/dl
Adverse reactions of oral iron Strategies to ↓ side effects include:
Upper gastrointestinal side effects: 1. ↓ dose (e.g., single 325-mg tablet of
Nausea, heartburn, epigastric pain → Fe2+ sulfate)
more dose dependent 2. Administering iron with meals
3. Use of enteric-coated preparations
Lower gastrointestinal side effects: (Ferrograd) or a polysaccharide-iron
Constipation or diarrhea, and dark complex
stools→ less related to dosing However, all these strategies ↓ iron
absorption
| P a g e 178