Page 28 - Gastrointestinal Bleeding (Xuất huyết tiêu hóa)
P. 28
302 PART III Symptoms, Signs, and Biopsychosocial Issues
remain uncomplicated. Bleeding may occur from vessels at the actual rate of rebleeding appears to be lower. In a large prospec-
neck or base of a diverticulum. 261 In our experience with defin- tive cohort study of patients with documented colonic diverticular
itive diverticular hemorrhage (see later), bleeding was from the hemorrhage (definitive or presumptive) by our group, the overall
base in 52% and from the neck in 48% of diverticula. 262 rate of rebleeding was 18% in 4 years—9% from recurrent diver-
Diverticula are common in Western countries, with a fre- ticular hemorrhage and 9% from other GI sources. 262
quency of 50% in older adults. 263 By contrast, diverticula are
found in fewer than 1% of continental African and Asian popula- Endoscopic Stigmata
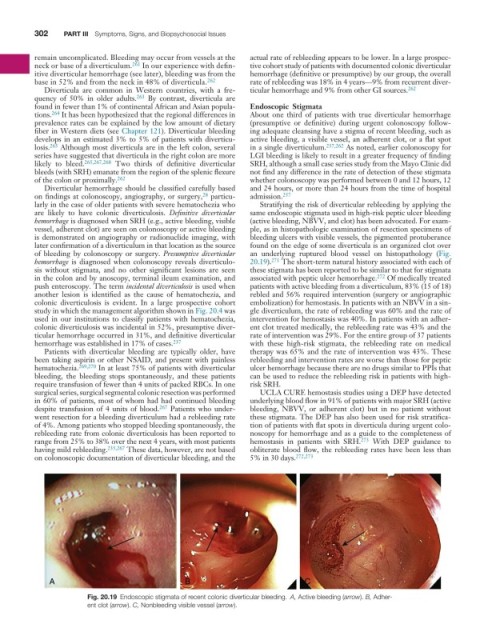
tions. 264 It has been hypothesized that the regional differences in About one third of patients with true diverticular hemorrhage
prevalence rates can be explained by the low amount of dietary (presumptive or definitive) during urgent colonoscopy follow-
fiber in Western diets (see Chapter 121). Diverticular bleeding ing adequate cleansing have a stigma of recent bleeding, such as
develops in an estimated 3% to 5% of patients with diverticu- active bleeding, a visible vessel, an adherent clot, or a flat spot
losis. 265 Although most diverticula are in the left colon, several in a single diverticulum. 237,262 As noted, earlier colonoscopy for
series have suggested that diverticula in the right colon are more LGI bleeding is likely to result in a greater frequency of finding
likely to bleed. 265,267,268 Two thirds of definitive diverticular SRH, although a small case series study from the Mayo Clinic did
bleeds (with SRH) emanate from the region of the splenic flexure not find any difference in the rate of detection of these stigmata
of the colon or proximally. 262 whether colonoscopy was performed between 0 and 12 hours, 12
Diverticular hemorrhage should be classified carefully based and 24 hours, or more than 24 hours from the time of hospital
on findings at colonoscopy, angiography, or surgery, particu- admission. 257
28
larly in the case of older patients with severe hematochezia who Stratifying the risk of diverticular rebleeding by applying the
are likely to have colonic diverticulosis. Definitive diverticular same endoscopic stigmata used in high-risk peptic ulcer bleeding
hemorrhage is diagnosed when SRH (e.g., active bleeding, visible (active bleeding, NBVV, and clot) has been advocated. For exam-
vessel, adherent clot) are seen on colonoscopy or active bleeding ple, as in histopathologic examination of resection specimens of
is demonstrated on angiography or radionuclide imaging, with bleeding ulcers with visible vessels, the pigmented protuberance
later confirmation of a diverticulum in that location as the source found on the edge of some diverticula is an organized clot over
of bleeding by colonoscopy or surgery. Presumptive diverticular an underlying ruptured blood vessel on histopathology (Fig.
hemorrhage is diagnosed when colonoscopy reveals diverticulo- 20.19). 271 The short-term natural history associated with each of
sis without stigmata, and no other significant lesions are seen these stigmata has been reported to be similar to that for stigmata
in the colon and by anoscopy, terminal ileum examination, and associated with peptic ulcer hemorrhage. 272 Of medically treated
push enteroscopy. The term incidental diverticulosis is used when patients with active bleeding from a diverticulum, 83% (15 of 18)
another lesion is identified as the cause of hematochezia, and rebled and 56% required intervention (surgery or angiographic
colonic diverticulosis is evident. In a large prospective cohort embolization) for hemostasis. In patients with an NBVV in a sin-
study in which the management algorithm shown in Fig. 20.4 was gle diverticulum, the rate of rebleeding was 60% and the rate of
used in our institutions to classify patients with hematochezia, intervention for hemostasis was 40%. In patients with an adher-
colonic diverticulosis was incidental in 52%, presumptive diver- ent clot treated medically, the rebleeding rate was 43% and the
ticular hemorrhage occurred in 31%, and definitive diverticular rate of intervention was 29%. For the entire group of 37 patients
hemorrhage was established in 17% of cases. 237 with these high-risk stigmata, the rebleeding rate on medical
Patients with diverticular bleeding are typically older, have therapy was 65% and the rate of intervention was 43%. These
been taking aspirin or other NSAID, and present with painless rebleeding and intervention rates are worse than those for peptic
hematochezia. 269,270 In at least 75% of patients with diverticular ulcer hemorrhage because there are no drugs similar to PPIs that
bleeding, the bleeding stops spontaneously, and these patients can be used to reduce the rebleeding risk in patients with high-
require transfusion of fewer than 4 units of packed RBCs. In one risk SRH.
surgical series, surgical segmental colonic resection was performed UCLA CURE hemostasis studies using a DEP have detected
in 60% of patients, most of whom had had continued bleeding underlying blood flow in 91% of patients with major SRH (active
despite transfusion of 4 units of blood. 267 Patients who under- bleeding, NBVV, or adherent clot) but in no patient without
went resection for a bleeding diverticulum had a rebleeding rate these stigmata. The DEP has also been used for risk stratifica-
of 4%. Among patients who stopped bleeding spontaneously, the tion of patients with flat spots in diverticula during urgent colo-
rebleeding rate from colonic diverticulosis has been reported to noscopy for hemorrhage and as a guide to the completeness of
range from 25% to 38% over the next 4 years, with most patients hemostasis in patients with SRH. 273 With DEP guidance to
having mild rebleeding. 235,267 These data, however, are not based obliterate blood flow, the rebleeding rates have been less than
on colonoscopic documentation of diverticular bleeding, and the 5% in 30 days. 272,273
A B C
Fig. 20.19 Endoscopic stigmata of recent colonic diverticular bleeding. A, Active bleeding (arrow). B, Adher-
ent clot (arrow). C, Nonbleeding visible vessel (arrow).