Page 31 - Gastrointestinal Bleeding (Xuất huyết tiêu hóa)
P. 31
CHAPTER 20 Gastrointestinal Bleeding 305
techniques. A topical calcium channel blocker (e.g., 2% topical
diltiazem cream) and control of constipation with fiber supple- 20
mentation and stool softeners plus sitz baths will heal most anal
fissures (see Chapter 129).
Rectal Varices
Ectopic varices may develop in the rectal mucosa between the
superior hemorrhoidal veins (portal circulation) and middle and
inferior hemorrhoidal veins (systemic circulation) in patients
with portal hypertension. On sigmoidoscopy, rectal varices
are seen during retroflexion as venous structures located sev-
eral centimeters above the dentate line and extending into the
rectum. They are distinct from internal hemorrhoids. The
frequency of rectal varices increases with the degree of portal
hypertension. Approximately 60% of patients with a history of
bleeding esophageal varices have rectal varices, but they are a
rare cause of severe hematochezia. 27,230,294 The treatment of
bleeding rectal varices is similar to that for esophageal varices,
with sclerotherapy, band ligation, or a portosystemic shunt (see
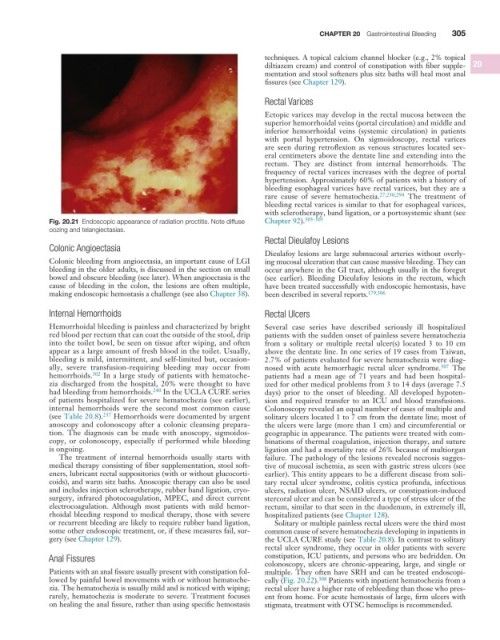
Fig. 20.21 Endoscopic appearance of radiation proctitis. Note diffuse Chapter 92). 303-305
oozing and telangiectasias.
Rectal Dieulafoy Lesions
Colonic Angioectasia
Dieulafoy lesions are large submucosal arteries without overly-
Colonic bleeding from angioectasia, an important cause of LGI ing mucosal ulceration that can cause massive bleeding. They can
bleeding in the older adults, is discussed in the section on small occur anywhere in the GI tract, although usually in the foregut
bowel and obscure bleeding (see later). When angioectasia is the (see earlier). Bleeding Dieulafoy lesions in the rectum, which
cause of bleeding in the colon, the lesions are often multiple, have been treated successfully with endoscopic hemostasis, have
making endoscopic hemostasis a challenge (see also Chapter 38). been described in several reports. 179,306
Internal Hemorrhoids Rectal Ulcers
Hemorrhoidal bleeding is painless and characterized by bright Several case series have described seriously ill hospitalized
red blood per rectum that can coat the outside of the stool, drip patients with the sudden onset of painless severe hematochezia
into the toilet bowl, be seen on tissue after wiping, and often from a solitary or multiple rectal ulcer(s) located 3 to 10 cm
appear as a large amount of fresh blood in the toilet. Usually, above the dentate line. In one series of 19 cases from Taiwan,
bleeding is mild, intermittent, and self-limited but, occasion- 2.7% of patients evaluated for severe hematochezia were diag-
ally, severe transfusion-requiring bleeding may occur from nosed with acute hemorrhagic rectal ulcer syndrome. 307 The
hemorrhoids. 302 In a large study of patients with hematoche- patients had a mean age of 71 years and had been hospital-
zia discharged from the hospital, 20% were thought to have ized for other medical problems from 3 to 14 days (average 7.5
had bleeding from hemorrhoids. 240 In the UCLA CURE series days) prior to the onset of bleeding. All developed hypoten-
of patients hospitalized for severe hematochezia (see earlier), sion and required transfer to an ICU and blood transfusions.
internal hemorrhoids were the second most common cause Colonoscopy revealed an equal number of cases of multiple and
(see Table 20.8). 237 Hemorrhoids were documented by urgent solitary ulcers located 1 to 7 cm from the dentate line; most of
anoscopy and colonoscopy after a colonic cleansing prepara- the ulcers were large (more than 1 cm) and circumferential or
tion. The diagnosis can be made with anoscopy, sigmoidos- geographic in appearance. The patients were treated with com-
copy, or colonoscopy, especially if performed while bleeding binations of thermal coagulation, injection therapy, and suture
is ongoing. ligation and had a mortality rate of 26% because of multiorgan
The treatment of internal hemorrhoids usually starts with failure. The pathology of the lesions revealed necrosis sugges-
medical therapy consisting of fiber supplementation, stool soft- tive of mucosal ischemia, as seen with gastric stress ulcers (see
eners, lubricant rectal suppositories (with or without glucocorti- earlier). This entity appears to be a different disease from soli-
coids), and warm sitz baths. Anoscopic therapy can also be used tary rectal ulcer syndrome, colitis cystica profunda, infectious
and includes injection sclerotherapy, rubber band ligation, cryo- ulcers, radiation ulcer, NSAID ulcers, or constipation-induced
surgery, infrared photocoagulation, MPEC, and direct current stercoral ulcer and can be considered a type of stress ulcer of the
electrocoagulation. Although most patients with mild hemor- rectum, similar to that seen in the duodenum, in extremely ill,
rhoidal bleeding respond to medical therapy, those with severe hospitalized patients (see Chapter 128).
or recurrent bleeding are likely to require rubber band ligation, Solitary or multiple painless rectal ulcers were the third most
some other endoscopic treatment, or, if these measures fail, sur- common cause of severe hematochezia developing in inpatients in
gery (see Chapter 129). the UCLA CURE study (see Table 20.8). In contrast to solitary
rectal ulcer syndrome, they occur in older patients with severe
Anal Fissures constipation, ICU patients, and persons who are bedridden. On
colonoscopy, ulcers are chronic-appearing, large, and single or
Patients with an anal fissure usually present with constipation fol- multiple. They often have SRH and can be treated endoscopi-
lowed by painful bowel movements with or without hematoche- cally (Fig. 20.22). 308 Patients with inpatient hematochezia from a
zia. The hematochezia is usually mild and is noticed with wiping; rectal ulcer have a higher rate of rebleeding than those who pres-
rarely, hematochezia is moderate to severe. Treatment focuses ent from home. For acute hemostasis of large, firm ulcers with
on healing the anal fissure, rather than using specific hemostasis stigmata, treatment with OTSC hemoclips is recommended.