Page 10 - TCW_Benefit Guide_2019 FINAL
P. 10
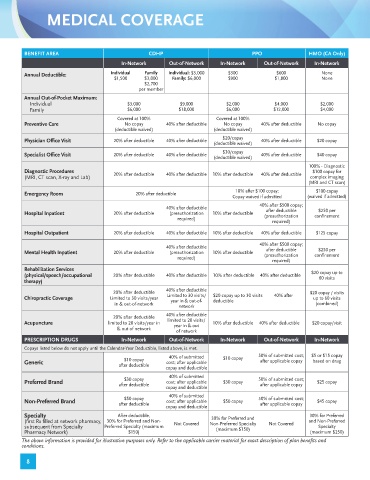
MEDICAL COVERAGE
BENEFIT AREA CDHP PPO HMO (CA Only)
In-Network Out-of-Network In-Network Out-of-Network In-Network
Annual Deductible: Individual Family Individual: $3,000 $300 $600 None
$1,500 $3,000 Family: $6,000 $900 $1,800 None
$2,700
per member
Annual Out-of-Pocket Maximum:
Individual $3,000 $9,000 $2,000 $4,000 $2,000
Family $6,000 $18,000 $6,000 $12,000 $4,000
Covered at 100% Covered at 100%
Preventive Care No copay 40% after deductible No copay 40% after deductible No copay
(deductible waived) (deductible waived)
$20/copay
Physician Office Visit 20% after deductible 40% after deductible 40% after deductible $20 copay
(deductible waived)
$30/copay
Specialist Office Visit 20% after deductible 40% after deductible 40% after deductible $40 copay
(deductible waived)
100% - Diagnostic
Diagnostic Procedures 20% after deductible 40% after deductible 10% after deductible 40% after deductible $100 copay for
(MRI, CT scan, X-ray and Lab) complex imaging
(MRI and CT scan)
10% after $100 copay; $100 copay
Emergency Room 20% after deductible
Copay waived if admitted (waived if admitted)
40% after $500 copay;
40% after deductible
$250 per
after deductible
Hospital Inpatient 20% after deductible (preauthorization 10% after deductible (preauthorization confinement
required)
required)
Hospital Outpatient 20% after deductible 40% after deductible 10% after deductible 40% after deductible $125 copay
40% after $500 copay;
40% after deductible after deductible $250 per
Mental Health Inpatient 20% after deductible (preauthorization 10% after deductible (preauthorization confinement
required)
required)
Rehabilitation Services $20 copay up to
(physical/speech/occupational 20% after deductible 40% after deductible 10% after deductible 40% after deductible 60 visits
therapy)
40% after deductible
20% after deductible $20 copay / visits
Chiropractic Coverage Limited to 30 visits/year Limited to 30 visits/ $20 copay up to 30 visits 40% after up to 60 visits
deductible
year in & out-of-
in & out-of-network (combined)
network
40% after deductible
20% after deductible
Acupuncture limited to 20 visits/year in limited to 20 visits/ 10% after deductible 40% after deductible $20 copay/visit
year in & out
& out of network
of network
PRESCRIPTION DRUGS In-Network Out-of-Network In-Network Out-of-Network In-Network
Copays listed below do not apply until the Calendar-Year Deductible, listed above, is met.
40% of submitted 50% of submitted cost; $5 or $15 copay
$10 copay $10 copay after applicable copay based on drug
Generic cost; after applicable
after deductible
copay and deductible
40% of submitted
$30 copay 50% of submitted cost;
Preferred Brand cost; after applicable $30 copay $25 copay
after deductible after applicable copay
copay and deductible
40% of submitted
$50 copay 50% of submitted cost;
Non-Preferred Brand cost; after applicable $50 copay $45 copay
after deductible after applicable copay
copay and deductible
Specialty After deductible, 30% for Preferred and 30% for Preferred
(first Rx filled at network pharmacy, 30% for Preferred and Non- Not Covered Non-Preferred Specialty Not Covered and Non-Preferred
subsequent from Specialty Preferred Specialty (maximum (maximum $150) Specialty
Pharmacy Network) $150) (maximum $250)
The above information is provided for illustrative purposes only. Refer to the applicable carrier material for exact description of plan benefits and
conditions.
8