Page 13 - Hitachi Benefits Booklet Final
P. 13
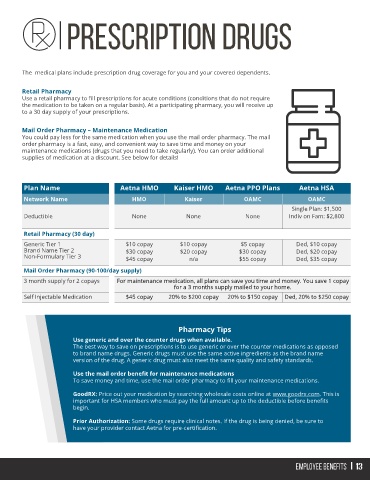
The medical plans include prescription drug coverage for you and your covered dependents.
Retail Pharmacy
Use a retail pharmacy to fill prescriptions for acute conditions (conditions that do not require
the medication to be taken on a regular basis). At a participating pharmacy, you will receive up
to a 30 day supply of your prescriptions.
Mail Order Pharmacy – Maintenance Medication
You could pay less for the same medication when you use the mail order pharmacy. The mail
order pharmacy is a fast, easy, and convenient way to save time and money on your
maintenance medications (drugs that you need to take regularly). You can order additional
supplies of medication at a discount. See below for details!
Plan Name Aetna HMO Kaiser HMO Aetna PPO Plans Aetna HSA
Network Name HMO Kaiser OAMC OAMC
Single Plan: $1,500
Deductible None None None Indiv on Fam: $2,800
Retail Pharmacy (30 day)
Generic Tier 1 $10 copay $10 copay $5 copay Ded, $10 copay
Brand Name Tier 2 $30 copay $20 copay $30 copay Ded, $20 copay
Non-Formulary Tier 3 $45 copay n/a $55 copay Ded, $35 copay
Mail Order Pharmacy (90-100/day supply)
3 month supply for 2 copays For maintenance medication, all plans can save you time and money. You save 1 copay
for a 3 months supply mailed to your home.
Self Injectable Medication $45 copay 20% to $200 copay 20% to $150 copay Ded, 20% to $250 copay
Pharmacy Tips
Use generic and over the counter drugs when available.
The best way to save on prescriptions is to use generic or over the counter medications as opposed
to brand name drugs. Generic drugs must use the same active ingredients as the brand name
version of the drug. A generic drug must also meet the same quality and safety standards.
Use the mail order benefit for maintenance medications
To save money and time, use the mail order pharmacy to fill your maintenance medications.
GoodRX: Price out your medication by searching wholesale costs online at www.goodrx.com. This is
important for HSA members who must pay the full amount up to the deductible before benefits
begin.
Prior Authorization: Some drugs require clinical notes. If the drug is being denied, be sure to
have your provider contact Aetna for pre-certification.