Page 13 - 2022 AEO Benefit Guide
P. 13
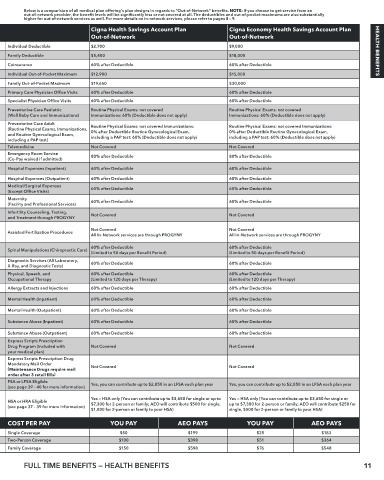
Below is a comparision of all medical plan offering’s plan designs in regards to “Out-of-Network” benefits. NOTE: If you choose to get service from an
out-of-network provider, the benefit levels will be significantly less or not covered at all. The deductibles and out-of-pocket maximums are also substantially
higher for out-of-network services as well. For more details on in-network services, please refer to pages 8 – 9.
Cigna Open Access Plus Plan Cigna Open Access Plus HRA Plan Cigna Health Savings Account Plan Cigna Economy Health Savings Account Plan
Out-of-Network Out-of-Network Out-of-Network Out-of-Network
Individual Deductible $1,000 $4,000 Individual Deductible $2,700 $9,000
Family Deductible $3,000 $8,000 Family Deductible $5,400 $18,000 HEALTH BENEFITS
Coinsurance 60% after Deductible 60% after Deductible Coinsurance 60% after Deductible 60% after Deductible
Individual Out-of-Pocket Maximum $10,000 $15,000 Individual Out-of-Pocket Maximum $12,900 $15,000
Family Out-of-Pocket Maximum $20,000 $30,000 Family Out-of-Pocket Maximum $19,650 $30,000
Primary Care Physician Office Visits 60% after Deductible 70% after Deductible Primary Care Physician Office Visits 60% after Deductible 60% after Deductible
Specialist Physician Office Visits 60% after Deductible 70% after Deductible Specialist Physician Office Visits 60% after Deductible 60% after Deductible
Preventative Care Pediatric 60% after Deductible Routine Physical Exams: not covered Preventative Care Pediatric Routine Physical Exams: not covered Routine Physical Exams: not covered
(Well Baby Care and Immunizations) (Routine Physical Exams not covered) Immunizations: 60% after Deductible (Well Baby Care and Immunizations) Immunizations: 60% (Deductible does not apply) Immunizations: 60% (Deductible does not apply)
Preventative Care Adult Preventative Care Adult Routine Physical Exams: not covered Immunizations: Routine Physical Exams: not covered Immunizations:
(Routine Physical Exams, Immunizations, 60% after Deductible 60% after Deductible (Routine Physical Exams, Immunizations, 0% after Deductible Routine Gynecological Exam, 0% after Deductible Routine Gynecological Exam,
and Routine Gynecological Exam, (Routine Physical Exams not covered) (Routine Physical Exams: not covered) and Routine Gynecological Exam, including a PAP test: 60% (Deductible does not apply) including a PAP test: 60% (Deductible does not apply)
including a PAP test) including a PAP test)
Telemedicine Not Covered Not Covered Telemedicine Not Covered Not Covered
Emergency Room Service Emergency Room Service
(Co-Pay waived if admitted) 80% after $250 Co-Pay (Deductible does not apply) 80% after $250 Co-Pay (Deductible does not apply) (Co-Pay waived if admitted) 80% after Deductible 80% after Deductible
60% after Deductible
Hospital Expenses (Inpatient) 60% after Deductible Hospital Expenses (Inpatient) 60% after Deductible 60% after Deductible
(Limit of 90 days per Benefit Period)
Hospital Expenses (Outpatient) 60% after Deductible 60% after Deductible Hospital Expenses (Outpatient) 60% after Deductible 60% after Deductible
Medical/Surgical Expenses 60% after Deductible 60% after Deductible Medical/Surgical Expenses 60% after Deductible 60% after Deductible
(Except Office Visits) (Except Office Visits)
Maternity 60% after Deductible 60% after Deductible Maternity 60% after Deductible 60% after Deductible
(Facility and Professional Services) (Facility and Professional Services)
Infertility Counseling, Testing, Not Covered Not Covered Infertility Counseling, Testing, Not Covered Not Covered
and Treatment through PROGYNY and Treatment through PROGYNY
Not Covered Not Covered Not Covered Not Covered
Assisted Fertilization Procedures Assisted Fertilization Procedures
All In-Network services are through PROGYNY All In-Network services are through PROGYNY All In-Network services are through PROGYNY All In-Network services are through PROGYNY
60% after Deductible 60% after Deductible 60% after Deductible 60% after Deductible
Spinal Manipulations (Chiropractic Care) Spinal Manipulations (Chiropractic Care)
(Limited to 50 days per Benefit Period) (Limited to 50 days per Benefit Period) (Limited to 50 days per Benefit Period) (Limited to 50 days per Benefit Period)
Diagnostic Services (All Laboratory, 60% after Deductible 60% after Deductible Diagnostic Services (All Laboratory, 60% after Deductible 60% after Deductible
X-Ray, and Diagnostic Tests) X-Ray, and Diagnostic Tests)
Physical, Speech, and 60% after Deductible 60% after Deductible Physical, Speech, and 60% after Deductible 60% after Deductible
Occupational Therapy (Limited to 120 days per Therapy) (Limited to 120 days per Therapy) Occupational Therapy (Limited to 120 days per Therapy) (Limited to 120 days per Therapy)
Allergy Extracts and Injections 60% after Deductible 60% after Deductible Allergy Extracts and Injections 60% after Deductible 60% after Deductible
60% after Deductible
Mental Health (Inpatient) 60% after Deductible Mental Health (Inpatient) 60% after Deductible 60% after Deductible
(Limit of 90 days per Benefit Period)
Mental Health (Outpatient) 60% after Deductible 70% after Deductible Mental Health (Outpatient) 60% after Deductible 60% after Deductible
60% after Deductible
Substance Abuse (Inpatient) 60% after Deductible Substance Abuse (Inpatient) 60% after Deductible 60% after Deductible
(Limit of 90 days per Benefit Period)
Substance Abuse (Outpatient) 60% after Deductible 70% after Deductible Substance Abuse (Outpatient) 60% after Deductible 60% after Deductible
Express Scripts Prescription Express Scripts Prescription
Drug Program (included with Not Covered Not Covered Drug Program (included with Not Covered Not Covered
your medical plan) your medical plan)
Express Scripts Prescription Drug Express Scripts Prescription Drug
Mandatory Mail Order Mandatory Mail Order
( Maintenance Drugs require mail Not Covered Not Covered ( Maintenance Drugs require mail Not Covered Not Covered
order after 3 retail fills ) order after 3 retail fills )
FSA or LFSA Eligible Yes, you can contribute up to $2,850 into an FSA for each Yes, you can contribute up to $2,850 into an FSA for each plan year FSA or LFSA Eligible Yes, you can contribute up to $2,850 in an LFSA each plan year Yes, you can contribute up to $2,850 in an LFSA each plan year
(see page 39 – 40 for more information) plan year (see page 39 – 40 for more information)
Yes — HRA only (AEO will contribute $500 for single, $1,000 for
HSA or HRA Eligible No (You are not eligible for an HSA or HRA) family into your Health Reimbursement Account — HRA — each HSA or HRA Eligible Yes — HSA only (You can contribute up to $3,650 for single or up to Yes — HSA only (You can contribute up to $3,650 for single or
up to $7,300 for 2-person or family; AEO will contribute $250 for
$7,300 for 2-person or family; AEO will contribute $500 for single,
(see page 37 – 39 for more information) year you are enrolled, up to a maximum balance of (see page 37 – 39 for more information) $1,000 for 2-person or family to your HSA) single, $500 for 2-person or family to your HSA)
$2,500/single or $5,000/family.)
COST PER PAY YOU PAY AEO PAYS YOU PAY AEO PAYS COST PER PAY YOU PAY AEO PAYS YOU PAY AEO PAYS
Single Coverage $84 $177 $39 $197 Single Coverage $50 $199 $25 $183
Two-Person Coverage $167 $354 $78 $394 Two-Person Coverage $100 $398 $51 $364
Family Coverage $251 $532 $117 $593 Family Coverage $150 $598 $76 $548
FULL TIME BENEFITS — HEALTH BENEFITS 11