Page 96 - Sách năm 2022 - Fulltext - hieu final
P. 96
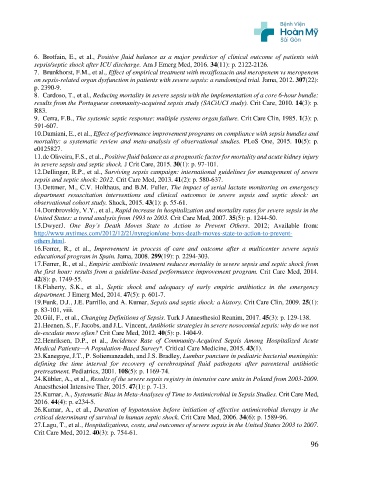
6. Brotfain, E., et al., Positive fluid balance as a major predictor of clinical outcome of patients with
sepsis/septic shock after ICU discharge. Am J Emerg Med, 2016. 34(11): p. 2122-2126.
7. Brunkhorst, F.M., et al., Effect of empirical treatment with moxifloxacin and meropenem vs meropenem
on sepsis-related organ dysfunction in patients with severe sepsis: a randomized trial. Jama, 2012. 307(22):
p. 2390-9.
8. Cardoso, T., et al., Reducing mortality in severe sepsis with the implementation of a core 6-hour bundle:
results from the Portuguese community-acquired sepsis study (SACiUCI study). Crit Care, 2010. 14(3): p.
R83.
9. Cerra, F.B., The systemic septic response: multiple systems organ failure. Crit Care Clin, 1985. 1(3): p.
591-607.
10. Damiani, E., et al., Effect of performance improvement programs on compliance with sepsis bundles and
mortality: a systematic review and meta-analysis of observational studies. PLoS One, 2015. 10(5): p.
e0125827.
11. de Oliveira, F.S., et al., Positive fluid balance as a prognostic factor for mortality and acute kidney injury
in severe sepsis and septic shock. J Crit Care, 2015. 30(1): p. 97-101.
12. Dellinger, R.P., et al., Surviving sepsis campaign: international guidelines for management of severe
sepsis and septic shock: 2012. Crit Care Med, 2013. 41(2): p. 580-637.
13. Dettmer, M., C.V. Holthaus, and B.M. Fuller, The impact of serial lactate monitoring on emergency
department resuscitation interventions and clinical outcomes in severe sepsis and septic shock: an
observational cohort study. Shock, 2015. 43(1): p. 55-61.
14. Dombrovskiy, V.Y., et al., Rapid increase in hospitalization and mortality rates for severe sepsis in the
United States: a trend analysis from 1993 to 2003. Crit Care Med, 2007. 35(5): p. 1244-50.
15. DwyerJ. One Boy’s Death Moves State to Action to Prevent Others. 2012; Available from:
http://www.nytimes.com/2012/12/21/nyregion/one-boys-death-moves-state-to-action-to-prevent-
others.html.
16. Ferrer, R., et al., Improvement in process of care and outcome after a multicenter severe sepsis
educational program in Spain. Jama, 2008. 299(19): p. 2294-303.
17. Ferrer, R., et al., Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from
the first hour: results from a guideline-based performance improvement program. Crit Care Med, 2014.
42(8): p. 1749-55.
18. Flaherty, S.K., et al., Septic shock and adequacy of early empiric antibiotics in the emergency
department. J Emerg Med, 2014. 47(5): p. 601-7.
19. Funk, D.J., J.E. Parrillo, and A. Kumar, Sepsis and septic shock: a history. Crit Care Clin, 2009. 25(1):
p. 83-101, viii.
20. Gül, F., et al., Changing Definitions of Sepsis. Turk J Anaesthesiol Reanim, 2017. 45(3): p. 129-138.
21. Heenen, S., F. Jacobs, and J.L. Vincent, Antibiotic strategies in severe nosocomial sepsis: why do we not
de-escalate more often? Crit Care Med, 2012. 40(5): p. 1404-9.
22. Henriksen, D.P., et al., Incidence Rate of Community-Acquired Sepsis Among Hospitalized Acute
Medical Patients—A Population-Based Survey*. Critical Care Medicine, 2015. 43(1).
23. Kanegaye, J.T., P. Soliemanzadeh, and J.S. Bradley, Lumbar puncture in pediatric bacterial meningitis:
defining the time interval for recovery of cerebrospinal fluid pathogens after parenteral antibiotic
pretreatment. Pediatrics, 2001. 108(5): p. 1169-74.
24. Kübler, A., et al., Results of the severe sepsis registry in intensive care units in Poland from 2003-2009.
Anaesthesiol Intensive Ther, 2015. 47(1): p. 7-13.
25. Kumar, A., Systematic Bias in Meta-Analyses of Time to Antimicrobial in Sepsis Studies. Crit Care Med,
2016. 44(4): p. e234-5.
26. Kumar, A., et al., Duration of hypotension before initiation of effective antimicrobial therapy is the
critical determinant of survival in human septic shock. Crit Care Med, 2006. 34(6): p. 1589-96.
27. Lagu, T., et al., Hospitalizations, costs, and outcomes of severe sepsis in the United States 2003 to 2007.
Crit Care Med, 2012. 40(3): p. 754-61.
96