Page 219 - Feline Cardiology
P. 219
224 Section F: Arrhythmias and Other Electrocardiographic Abnormalities
suppression of sinus tachycardia could cause hemody- (regular formulation) 7.5 mg PO q 8h, or sotalol 2 mg/kg
namic collapse; 2) with AT confirmed, determine whether PO q 12h. Sustained-release diltiazem (Cardizem-CD,
AT alone appears responsible for the unstable state, Dilacor-XL) is not recommended in cats due to unpre-
which mainly depends on the heart rate (is it >260 beats/ dictable bioavailability and toxicosis (Johnson et al.
minute?). If so, identify and correct systemic abnormali- 1996; Wall et al. 2005).
ties that increase sympathetic tone (hypovolemia, With either acute (IV) or chronic (PO) treatment, the
anemia, hypoxemia, etc.); 3) in an unstable cat with con- therapeutic goal is to reduce or eliminate extremes of
firmed AT at a rate >260/minute and in whom extracar- tachycardia that would reduce cardiac output—i.e., to
diac disorders are controlled or absent, intravenous provide medication at a level that prevents HR >260 and
diltiazem (0.125 mg/kg IV infusion over 1 minute), pro- stops AT-associated syncope or other arrhythmia-
pranolol (0.1 mg total bolus/cat, once), or esmolol 25– associated clinical signs if present. Pharmacologically
200 mcg/kg/min intravenous infusion (begin low and forcing the heart rate beyond these parameters and into
gradually increase to achieve desired effect) may be the range of normal sinus rhythm (110–180 beats/
administered with continuous ECG monitoring. The minute) would likely require excessive dosages of medi-
time to effect for any of these drugs is typically <2 cation and is not recommended.
Follow-up is warranted after 7–14 days of antiar-
minutes, and a decrease of 5–20% in heart rate is consid- rhythmic therapy, or sooner if clinical signs worsen or
Arrhythmias change, or an improvement, in the cat’s demeanor, pulse new clinical signs appear. Such follow-up should consist
ered a satisfactory response, together with either no
of physical exam, 10-lead resting ECG, and repetition of
strength, and other hemodynamic parameters. If no
effect is seen, the dose can be increased (esmolol) or
malities if they were noted.
repeated twice in 10 minutes (diltiazem, propranolol). If laboratory tests as indicated to evaluate ongoing abnor-
this approach remains ineffective, the diagnosis should Atrial tachycardia does not clearly confer a worse
be questioned (repeat 10-lead ECG, including with a prognosis, and the prognosis for cats with AT is not
vagal maneuver) and logistical errors should be sought distinguishable from the prognosis of its underlying dis-
and corrected (is the IV catheter patent?) before addi- orders (cardiomyopathy, hyperthyroidism, others) when
tional doses are considered. A cat with AT that is stable AT is absent.
(conscious, breathing comfortably, fair or good pulse
strength) at the time of evaluation may be treated with Atrial Fibrillation
atenolol 6.25 mg PO q 12h; uptitration to 12.5 mg PO q Atrial fibrillation (AF) is said to represent a state of
12h is a robust increase that may be considered after electrical chaos in the atria. The atria depolarize from
several days if AT persists. This higher dosage has multiple foci at a rate of several hundred impulses per
been used by some cardiologists but may be excessive minute, many or most of which never cross the AV node
(causing inappetence, lethargy, and weakness) in some to the ventricles. The result is a heart rate that varies
cats, particularly if there is concurrent structural cardiac from normal to elevated (e.g., 260/minute) and an irreg-
disease or other illness. Dilated cardiomyopathy is a rela- ular rhythm due to the patternless selection of impulses
tive contraindication, especially to the higher dosages. that are admitted through the AV node to the ventricles
Alternatives to atenolol include diltiazem hydrochloride (Figure 18.9).
QRS
T T
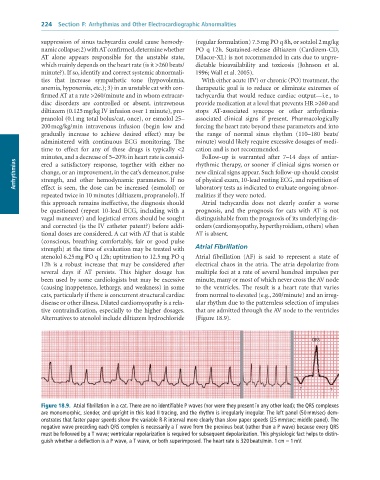
Figure 18.9. Atrial fibrillation in a cat. There are no identifiable P waves (nor were they present in any other lead); the QRS complexes
are monomorphic, slender, and upright in this lead II tracing, and the rhythm is irregularly irregular. The left panel (50 mm/sec) dem-
onstrates that faster paper speeds show the variable R-R interval more clearly than slow paper speeds (25 mm/sec; middle panel). The
negative wave preceding each QRS complex is necessarily a T wave from the previous beat (rather than a P wave) because every QRS
must be followed by a T wave; ventricular repolarization is required for subsequent depolarization. This physiologic fact helps to distin-
guish whether a deflection is a P wave, a T wave, or both superimposed. The heart rate is 320 beats/min. 1 cm = 1 mV.