Page 10 - T:\HR\Div\Employee Services (Cust_None)\Flipbuilder\Benefits Resource Guide FB Project\
P. 10
Medical, vision & pharmacy benefits, cont.
To use the mail order program, ask your physician to write a prescription for a
90-day supply with refills (as appropriate) and send it to Express Scripts.
Otherwise, obtain the order a mail order form from Express-Scripts.com and
follow the instructions for mailing your prescriptions and copayment to
Express Scripts.
Prescription medication tiers
Express Script’s categorizes prescription medications as Tier 1 (generic), Tier 2
(preferred brand), or Tier 3 (non-preferred brand). The cost of the medication
is not a primary factor in its tier classification. The tier classification of a
medication may change periodically. You can find up-to-date prescription
medication tiers on Express-Scripts.com; by using the Express Scripts mobile
app, or by contacting Express Scripts’ customer service.
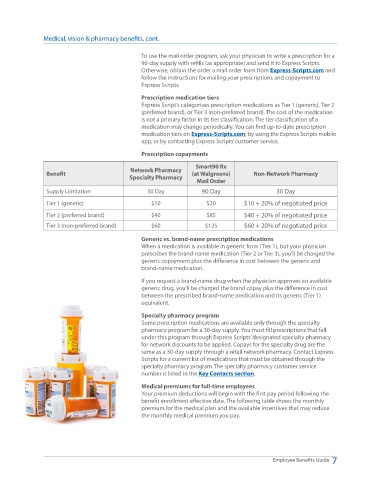
Prescription copayments
Smart90 Rx
Network Pharmacy
Benefit (at Walgreens) Non-Network Pharmacy
Specialty Pharmacy
Mail Order
Supply Limitation 30 Day 90 Day 30 Day
Tier 1 (generic) $10 $20 $10 + 20% of negotiated price
Tier 2 (preferred brand) $40 $85 $40 + 20% of negotiated price
Tier 3 (non-preferred brand) $60 $125 $60 + 20% of negotiated price
Generic vs. brand-name prescription medications
When a medication is available in generic form (Tier 1), but your physician
prescribes the brand-name medication (Tier 2 or Tier 3), you’ll be charged the
generic copayment plus the difference in cost between the generic and
brand-name medication.
If you request a brand-name drug when the physician approves an available
generic drug, you’ll be charged the brand copay plus the difference in cost
between the prescribed brand-name medication and its generic (Tier 1)
equivalent.
Specialty pharmacy program
Some prescription medications are available only through the specialty
pharmacy program for a 30-day supply. You must fill prescriptions that fall
under this program through Express Scripts’ designated specialty pharmacy
for network discounts to be applied. Copays for the specialty drug are the
same as a 30-day supply through a retail network pharmacy. Contact Express
Scripts for a current list of medications that must be obtained through the
specialty pharmacy program. The specialty pharmacy customer service
number is listed in the Key Contacts section.
Medical premiums for full-time employees
Your premium deductions will begin with the first pay period following the
benefit enrollment effective date. The following table shows the monthly
premium for the medical plan and the available incentives that may reduce
the monthly medical premium you pay.
Employee Benefits Guide 7