Page 18 - 2018 Zumba Employee Benefits Guide
P. 18
18
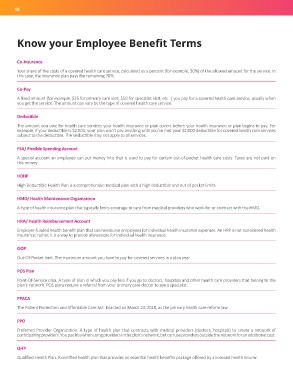
Know your Employee Benefit Terms
Co-Insurance
Your share of the costs of a covered health care service, calculated as a percent (for example, 30%) of the allowed amount for the service. In
this case, the insurance plan pays the remaining 70%.
Co-Pay
A fixed amount (for example, $25 for primary care visit; $50 for specialist visit, etc...) you pay for a covered health care service, usually when
you get the service. The amount can vary by the type of covered health care service.
Deductible
The amount you owe for health care services your health insurance or plan covers before your health insurance or plan begins to pay. For
example, if your deductible is $2,000, your plan won’t pay anything until you’ve met your $2,000 deductible for covered health care services
subject to the deductible. The deductible may not apply to all services.
FSA/ Flexible Spending Account
A special account an employee can put money into that is used to pay for certain out-of-pocket health care costs. Taxes are not paid on
this money.
HDHP
High Deductible Health Plan is a comprehensive medical plan with a high deductible and out of pocket limits.
HMO/ Health Maintenance Organization
A type of health insurance plan that typically limits coverage to care from medical providers who work for or contract with the HMO.
HRA/ Health Reimbursement Account
Employer-funded health benefit plan that can reimburse employees for individual health insurance expenses. An HRP is not considered health
insurance; rather, it is a way to provide allowances for individual health insurance.
OOP
Out-Of-Pocket limit. The maximum amount you have to pay for covered services in a plan year.
POS Plan
Point-Of-Service plan. A type of plan in which you pay less if you go to doctors, hospitals and other health care providers that belong to the
plan’s network. POS plans require a referral from your primary care doctor to see a specialist.
PPACA
The Patient Protection and Affordable Care Act. Enacted on March 23, 2010, as the primary health care reform law.
PPO
Preferred Provider Organization. A type of health plan that contracts with medical providers (doctors, hospitals) to create a network of
participating providers. You pay less when using providers in the plan’s network, but can use providers outside the network for an additional cost.
QHP
Qualified Health Plan. A certified health plan that provides an essential health benefits package offered by a licensed health insurer.