Page 73 - Rehab 2020
P. 73
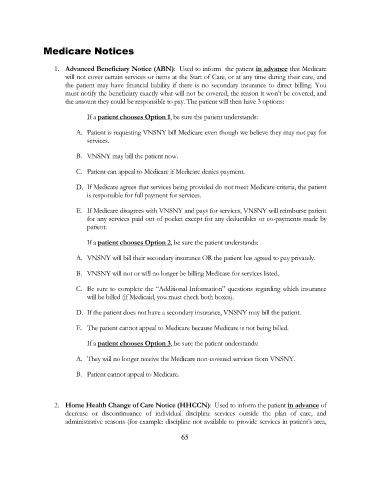
Medicare Notices
1. Advanced Beneficiary Notice (ABN): Used to inform the patient in advance that Medicare
will not cover certain services or items at the Start of Care, or at any time during their care, and
the patient may have financial liability if there is no secondary insurance to direct billing. You
must notify the beneficiary exactly what will not be covered, the reason it won’t be covered, and
the amount they could be responsible to pay. The patient will then have 3 options:
If a patient chooses Option 1, be sure the patient understands:
A. Patient is requesting VNSNY bill Medicare even though we believe they may not pay for
services.
B. VNSNY may bill the patient now.
C. Patient can appeal to Medicare if Medicare denies payment.
D. If Medicare agrees that services being provided do not meet Medicare criteria, the patient
is responsible for full payment for services.
E. If Medicare disagrees with VNSNY and pays for services, VNSNY will reimburse patient
for any services paid out of pocket except for any deductibles or co-payments made by
patient.
If a patient chooses Option 2, be sure the patient understands:
A. VNSNY will bill their secondary insurance OR the patient has agreed to pay privately.
B. VNSNY will not or will no longer be billing Medicare for services listed.
C. Be sure to complete the “Additional Information” questions regarding which insurance
will be billed (if Medicaid, you must check both boxes).
D. If the patient does not have a secondary insurance, VNSNY may bill the patient.
E. The patient cannot appeal to Medicare because Medicare is not being billed.
If a patient chooses Option 3, be sure the patient understands:
A. They will no longer receive the Medicare non-covered services from VNSNY.
B. Patient cannot appeal to Medicare.
2. Home Health Change of Care Notice (HHCCN): Used to inform the patient in advance of
decrease or discontinuance of individual discipline services outside the plan of care, and
administrative reasons (for example: discipline not available to provide services in patient’s area,
65