Page 2483 - Cote clinical veterinary advisor dogs and cats 4th
P. 2483
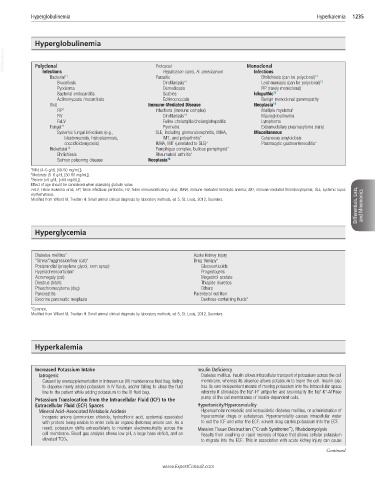
Hyperglobulinemia Hyperkalemia 1235
Hyperglobulinemia
VetBooks.ir Polyclonal Protozoal Monoclonal
Infections
Hepatozoon canis, H. americanum
Ehrlichiosis (can be polyclonal)
Bacterial* † Parasitic Infections †‡
Brucellosis Dirofilariasis* † Leishmaniasis (can be polyclonal) †‡
Pyoderma Demodicosis FIP (rarely monoclonal)
Bacterial endocarditis Scabies Idiopathic †‡
Actinomycosis /nocardiosis Echinococcosis Benign monoclonal gammopathy
Viral Immune-Mediated Disease Neoplasia †‡
FIP ‡ Infections (immune complex) Multiple myeloma ‡
FIV Dirofilariasis* † Macroglobulinemia
FeLV Feline cholangitis/cholangiohepatitis Lymphoma
Fungal* † Pyometra Extramedullary plasmacytoma (rare)
Systemic fungal infections (e.g., SLE, including glomerulonephritis, IMHA, Miscellaneous
blastomycosis, histoplasmosis, IMT, and polyarthritis* Cutaneous amyloidosis
coccidioidomycosis) IMHA, IMT (unrelated to SLE)* Plasmacytic gastroenterocolitis*
Rickettsial †‡ Pemphigus complex, bullous pemphigoid*
Ehrlichiosis Rheumatoid arthritis*
Salmon poisoning disease Neoplasia †‡
*Mild (4–5 g/dL [40-50 mg/mL]).
† Moderate (5–6 g/dL [50-60 mg/mL]).
‡ Severe (>6 g/dL [>60 mg/mL]).
Effect of age should be considered when assessing globulin value.
Differentials, Lists, and Mnemonics
FeLV, Feline leukemia virus; FIP, feline infectious peritonitis; FIV, feline immunodeficiency virus; IMHA, immune-mediated hemolytic anemia; IMT, immune-mediated thrombocytopenia; SLE, systemic lupus
erythematosus.
Modified from Willard M, Tvedten H: Small animal clinical diagnosis by laboratory methods, ed 5, St. Louis, 2012, Saunders.
Hyperglycemia
Diabetes mellitus* Acute kidney injury
“Stress”/aggression/fear (cat)* Drug therapy*
Postprandial (propylene glycol, corn syrup) Glucocorticoids
Hyperadrenocorticism* Progestogens
Acromegaly (cat) Megestrol acetate
Diestrus (bitch) Thiazide diuretics
Pheochromocytoma (dog) Others
Pancreatitis Parenteral nutrition
Exocrine pancreatic neoplasia Dextrose-containing fluids*
*Common.
Modified from Willard M, Tvedten H: Small animal clinical diagnosis by laboratory methods, ed 5, St. Louis, 2012, Saunders.
Hyperkalemia
Increased Potassium Intake Insulin Deficiency
Iatrogenic Diabetes mellitus. Insulin allows intracellular transport of potassium across the cell
Caused by oversupplementation in intravenous (IV) maintenance fluid bag, failing membrane, whereas its absence allows potassium to leave the cell. Insulin also
to disperse newly added potassium in IV fluids, and/or failing to close the fluid has its own independent means of moving potassium into the intracellular space
+
+
+
+
line to the patient while adding potassium to the IV fluid bag. whereby it stimulates the Na -H antiporter and secondarily the Na -K -ATPase
Potassium Translocation from the Intracellular Fluid (ICF) to the pump at the cell membranes of insulin-dependent cells.
Extracellular Fluid (ECF) Spaces Hypertonicity/Hyperosmolality
Mineral Acid–Associated Metabolic Acidosis Hyperosmolar nonketotic and ketoacidotic diabetes mellitus, or administration of
Inorganic anions (ammonium chloride, hydrochloric acid, azotemia) associated hyperosmolar drugs or substances. Hyperosmolality causes intracellular water
with protons being unable to enter cells as organic (ketones) anions can. As a to exit the ICF and enter the ECF; solvent drag carries potassium into the ECF.
result, potassium shifts extracellularly to maintain electroneutrality across the Massive Tissue Destruction (“Crush Syndrome”), Rhabdomyolysis
cell membrane. Blood gas analysis shows low pH, a large base deficit, and an Results from crushing or rapid necrosis of tissue that allows cellular potassium
elevated TCO 2. to migrate into the ECF. This in association with acute kidney injury can cause
Continued
www.ExpertConsult.com