Page 592 - Small Animal Internal Medicine, 6th Edition
P. 592
564 PART IV Hepatobiliary and Exocrine Pancreatic Disorders
VetBooks.ir
A B 30 m
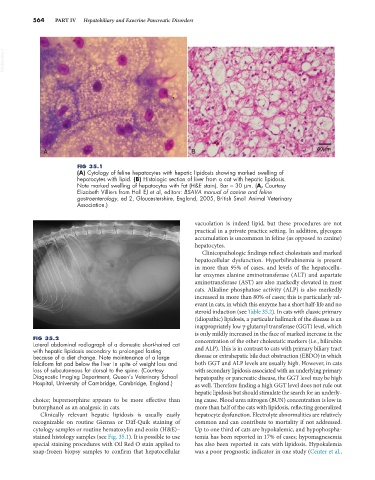
FIG 35.1
(A) Cytology of feline hepatocytes with hepatic lipidosis showing marked swelling of
hepatocytes with lipid. (B) Histologic section of liver from a cat with hepatic lipidosis.
Note marked swelling of hepatocytes with fat (H&E stain). Bar = 30 µm. (A, Courtesy
Elizabeth Villiers from Hall EJ et al, editors: BSAVA manual of canine and feline
gastroenterology, ed 2, Gloucestershire, England, 2005, British Small Animal Veterinary
Association.)
vacuolation is indeed lipid, but these procedures are not
practical in a private practice setting. In addition, glycogen
accumulation is uncommon in feline (as opposed to canine)
hepatocytes.
Clinicopathologic findings reflect cholestasis and marked
hepatocellular dysfunction. Hyperbilirubinemia is present
in more than 95% of cases, and levels of the hepatocellu-
lar enzymes alanine aminotransferase (ALT) and aspartate
aminotransferase (AST) are also markedly elevated in most
cats. Alkaline phosphatase activity (ALP) is also markedly
increased in more than 80% of cases; this is particularly rel-
evant in cats, in which this enzyme has a short half-life and no
steroid induction (see Table 35.2). In cats with classic primary
(idiopathic) lipidosis, a particular hallmark of the disease is an
inappropriately low γ-glutamyl transferase (GGT) level, which
is only mildly increased in the face of marked increase in the
FIG 35.2 concentration of the other cholestatic markers (i.e., bilirubin
Lateral abdominal radiograph of a domestic short-haired cat
with hepatic lipidosis secondary to prolonged fasting and ALP). This is in contrast to cats with primary biliary tract
because of a diet change. Note maintenance of a large disease or extrahepatic bile duct obstruction (EBDO) in which
falciform fat pad below the liver in spite of weight loss and both GGT and ALP levels are usually high. However, in cats
loss of subcutaneous fat dorsal to the spine. (Courtesy with secondary lipidosis associated with an underlying primary
Diagnostic Imaging Department, Queen’s Veterinary School hepatopathy or pancreatic disease, the GGT level may be high
Hospital, University of Cambridge, Cambridge, England.) as well. Therefore finding a high GGT level does not rule out
hepatic lipidosis but should stimulate the search for an underly-
choice; buprenorphine appears to be more effective than ing cause. Blood urea nitrogen (BUN) concentration is low in
butorphanol as an analgesic in cats. more than half of the cats with lipidosis, reflecting generalized
Clinically relevant hepatic lipidosis is usually easily hepatocyte dysfunction. Electrolyte abnormalities are relatively
recognizable on routine Giemsa or Diff-Quik staining of common and can contribute to mortality if not addressed.
cytology samples or routine hematoxylin and eosin (H&E)– Up to one third of cats are hypokalemic, and hypophospha-
stained histology samples (see Fig. 35.1). It is possible to use temia has been reported in 17% of cases; hypomagnesemia
special staining procedures with Oil Red O stain applied to has also been reported in cats with lipidosis. Hypokalemia
snap-frozen biopsy samples to confirm that hepatocellular was a poor prognostic indicator in one study (Center et al.,