Page 60 - R2P Front Desk Manual v1
P. 60
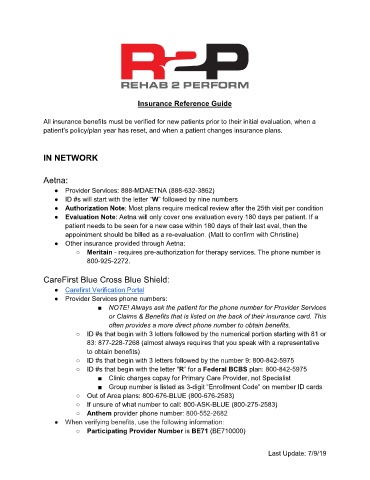
Insurance Reference Guide
All insurance benefits must be verified for new patients prior to their initial evaluation, when a
patient’s policy/plan year has reset, and when a patient changes insurance plans.
IN NETWORK
Aetna:
● Provider Services: 888-MDAETNA (888-632-3862)
● ID #s will start with the letter “W” followed by nine numbers
● Authorization Note: Most plans require medical review after the 25th visit per condition
● Evaluation Note: Aetna will only cover one evaluation every 180 days per patient. If a
patient needs to be seen for a new case within 180 days of their last eval, then the
appointment should be billed as a re-evaluation. (Matt to confirm with Christine)
● Other insurance provided through Aetna:
○ Meritain - requires pre-authorization for therapy services. The phone number is
800-925-2272.
CareFirst Blue Cross Blue Shield:
● Carefirst Verification Portal
● Provider Services phone numbers:
■ NOTE! Always ask the patient for the phone number for Provider Services
or Claims & Benefits that is listed on the back of their insurance card. This
often provides a more direct phone number to obtain benefits.
○ ID #s that begin with 3 letters followed by the numerical portion starting with 81 or
83: 877-228-7268 (almost always requires that you speak with a representative
to obtain benefits)
○ ID #s that begin with 3 letters followed by the number 9: 800-842-5975
○ ID #s that begin with the letter “R” for a Federal BCBS plan: 800-842-5975
■ Clinic charges copay for Primary Care Provider, not Specialist
■ Group number is listed as 3-digit “Enrollment Code” on member ID cards
○ Out of Area plans: 800-676-BLUE (800-676-2583)
○ If unsure of what number to call: 800-ASK-BLUE (800-275-2583)
○ Anthem provider phone number: 800-552-2682
● When verifying benefits, use the following information:
○ Participating Provider Number is BE71 (BE710000)
Last Update: 7/9/19