Page 8 - TruckPro-2022-Benefit Guide-FINAL
P. 8
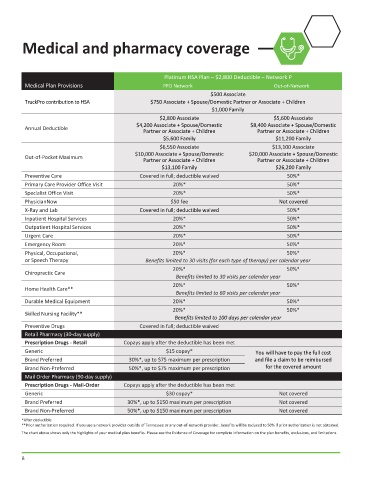
Medical and pharmacy coverage
Platinum HSA Plan – $2,800 Deductible – Network P
Medical Plan Provisions PPO Network Out-of-Network
$500 Associate
TruckPro contribution to HSA $750 Associate + Spouse/Domestic Partner or Associate + Children
$1,000 Family
$2,800 Associate $5,600 Associate
$4,200 Associate + Spouse/Domestic $8,400 Associate + Spouse/Domestic
Annual Deductible
Partner or Associate + Children Partner or Associate + Children
$5,600 Family $11,200 Family
$6,550 Associate $13,100 Associate
$10,000 Associate + Spouse/Domestic $20,000 Associate + Spouse/Domestic
Out-of-Pocket Maximum
Partner or Associate + Children Partner or Associate + Children
$13,100 Family $26,200 Family
Preventive Care Covered in full; deductible waived 50%*
Primary Care Provider Office Visit 20%* 50%*
Specialist Office Visit 20%* 50%*
PhysicianNow $50 fee Not covered
X-Ray and Lab Covered in full; deductible waived 50%*
Inpatient Hospital Services 20%* 50%*
Outpatient Hospital Services 20%* 50%*
Urgent Care 20%* 50%*
Emergency Room 20%* 50%*
Physical, Occupational, 20%* 50%*
or Speech Therapy Benefits limited to 30 visits (for each type of therapy) per calendar year
20%* 50%*
Chiropractic Care
Benefits limited to 30 visits per calendar year
20%* 50%*
Home Health Care**
Benefits limited to 60 visits per calendar year
Durable Medical Equipment 20%* 50%*
20%* 50%*
Skilled Nursing Facility**
Benefits limited to 100 days per calendar year
Preventive Drugs Covered in full; deductible waived
Retail Pharmacy (30-day supply)
Prescription Drugs - Retail Copays apply after the deductible has been met
Generic $15 copay* You will have to pay the full cost
Brand Preferred 30%*, up to $75 maximum per prescription and file a claim to be reimbursed
Brand Non-Preferred 50%*, up to $75 maximum per prescription for the covered amount
Mail Order Pharmacy (90-day supply)
Prescription Drugs - Mail-Order Copays apply after the deductible has been met
Generic $30 copay* Not covered
Brand Preferred 30%*, up to $150 maximum per prescription Not covered
Brand Non-Preferred 50%*, up to $150 maximum per prescription Not covered
*After deductible
**Prior authorization required. If you use a network provider outside of Tennessee or any out-of-network provider, benefits will be reduced to 50% if prior authorization is not obtained.
The chart above shows only the highlights of your medical plan benefits. Please see the Evidence of Coverage for complete information on the plan benefits, exclusions, and limitations.
8