Page 23 - 2021 Medical Plan SPD
P. 23
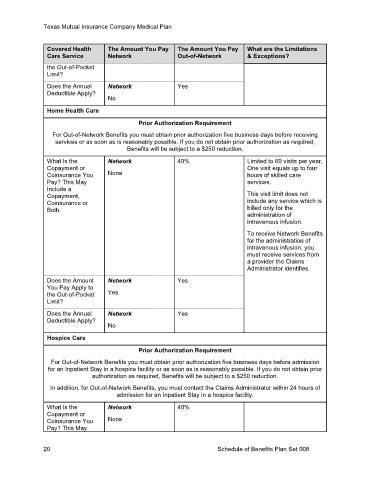
Texas Mutual Insurance Company Medical Plan
Covered Health The Amount You Pay The Amount You Pay What are the Limitations
Care Service Network Out-of-Network & Exceptions?
the Out-of-Pocket
Limit?
Does the Annual Network Yes
Deductible Apply?
No
Home Health Care
Prior Authorization Requirement
For Out-of-Network Benefits you must obtain prior authorization five business days before receiving
services or as soon as is reasonably possible. If you do not obtain prior authorization as required,
Benefits will be subject to a $250 reduction.
What Is the Network 40% Limited to 60 visits per year.
Copayment or One visit equals up to four
Coinsurance You None hours of skilled care
Pay? This May services.
Include a
Copayment, This visit limit does not
Coinsurance or include any service which is
Both. billed only for the
administration of
intravenous infusion.
To receive Network Benefits
for the administration of
intravenous infusion, you
must receive services from
a provider the Claims
Administrator identifies.
Does the Amount Network Yes
You Pay Apply to
the Out-of-Pocket Yes
Limit?
Does the Annual Network Yes
Deductible Apply?
No
Hospice Care
Prior Authorization Requirement
For Out-of-Network Benefits you must obtain prior authorization five business days before admission
for an Inpatient Stay in a hospice facility or as soon as is reasonably possible. If you do not obtain prior
authorization as required, Benefits will be subject to a $250 reduction.
In addition, for Out-of-Network Benefits, you must contact the Claims Administrator within 24 hours of
admission for an Inpatient Stay in a hospice facility.
What Is the Network 40%
Copayment or
Coinsurance You None
Pay? This May
20 Schedule of Benefits Plan Set 008