Page 24 - 2021 Medical Plan SPD
P. 24
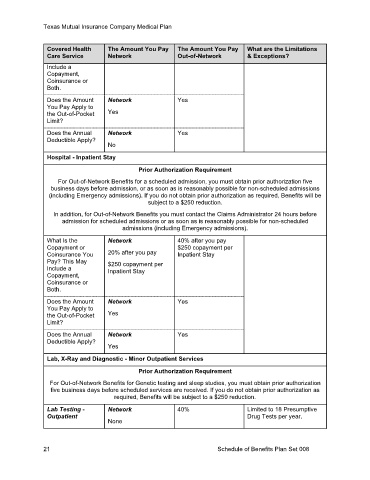
Texas Mutual Insurance Company Medical Plan
Covered Health The Amount You Pay The Amount You Pay What are the Limitations
Care Service Network Out-of-Network & Exceptions?
Include a
Copayment,
Coinsurance or
Both.
Does the Amount Network Yes
You Pay Apply to
the Out-of-Pocket Yes
Limit?
Does the Annual Network Yes
Deductible Apply?
No
Hospital - Inpatient Stay
Prior Authorization Requirement
For Out-of-Network Benefits for a scheduled admission, you must obtain prior authorization five
business days before admission, or as soon as is reasonably possible for non-scheduled admissions
(including Emergency admissions). If you do not obtain prior authorization as required, Benefits will be
subject to a $250 reduction.
In addition, for Out-of-Network Benefits you must contact the Claims Administrator 24 hours before
admission for scheduled admissions or as soon as is reasonably possible for non-scheduled
admissions (including Emergency admissions).
What Is the Network 40% after you pay
Copayment or $250 copayment per
Coinsurance You 20% after you pay Inpatient Stay
Pay? This May $250 copayment per
Include a Inpatient Stay
Copayment,
Coinsurance or
Both.
Does the Amount Network Yes
You Pay Apply to
the Out-of-Pocket Yes
Limit?
Does the Annual Network Yes
Deductible Apply?
Yes
Lab, X-Ray and Diagnostic - Minor Outpatient Services
Prior Authorization Requirement
For Out-of-Network Benefits for Genetic testing and sleep studies, you must obtain prior authorization
five business days before scheduled services are received. If you do not obtain prior authorization as
required, Benefits will be subject to a $250 reduction.
Lab Testing - Network 40% Limited to 18 Presumptive
Outpatient Drug Tests per year.
None
21 Schedule of Benefits Plan Set 008