Page 771 - Atlas of Histology with Functional Correlations
P. 771
inhibiting the resorptive action of osteoclasts, reducing calcium release, and
increasing calcium deposition in bones. Calcitonin also promotes excretion of
calcium and phosphate ions from the kidneys into the urine. The release of
calcitonin by the parafollicular cells depends on increased blood calcium
levels and is independent of the pituitary gland hormones. Thus, the release
of calcitonin is regulated by calcium levels through a simple feedback
mechanism.
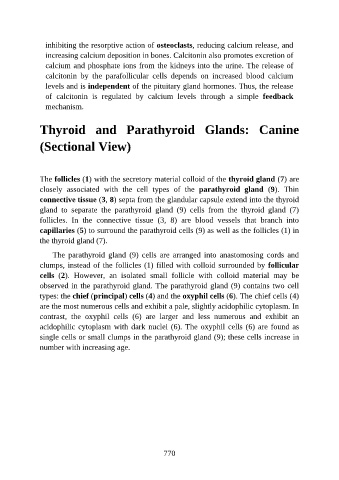
Thyroid and Parathyroid Glands: Canine
(Sectional View)
The follicles (1) with the secretory material colloid of the thyroid gland (7) are
closely associated with the cell types of the parathyroid gland (9). Thin
connective tissue (3, 8) septa from the glandular capsule extend into the thyroid
gland to separate the parathyroid gland (9) cells from the thyroid gland (7)
follicles. In the connective tissue (3, 8) are blood vessels that branch into
capillaries (5) to surround the parathyroid cells (9) as well as the follicles (1) in
the thyroid gland (7).
The parathyroid gland (9) cells are arranged into anastomosing cords and
clumps, instead of the follicles (1) filled with colloid surrounded by follicular
cells (2). However, an isolated small follicle with colloid material may be
observed in the parathyroid gland. The parathyroid gland (9) contains two cell
types: the chief (principal) cells (4) and the oxyphil cells (6). The chief cells (4)
are the most numerous cells and exhibit a pale, slightly acidophilic cytoplasm. In
contrast, the oxyphil cells (6) are larger and less numerous and exhibit an
acidophilic cytoplasm with dark nuclei (6). The oxyphil cells (6) are found as
single cells or small clumps in the parathyroid gland (9); these cells increase in
number with increasing age.
770