Page 131 - Fluid, Electrolyte, and Acid-Base Disorders in Small Animal Practice
P. 131
Disorders of Calcium: Hypercalcemia and Hypocalcemia 121
concentrations. Bone calcium mobilization is important
Parathyroid 433
gland in the acute regulation of blood calcium. Calcium
+ and phosphorus can be mobilized from calcium pho-
PTH PTH
sphate in the bone ECF compartment, but these stores
− Pi, Ca ++
Ca ++ − are rapidly depleted. The osteoblast is critical in limiting
the distribution of calcium and phosphate between bone
− and ECF, and exchangeable bone water is separated from
1,25(OH) D ECF water by the combined membranes of osteoblasts
2 3
+ lining bone surfaces. For greater or prolonged release
+ Ca ++
+ of calcium from bone, osteoclastic bone resorption must
be activated. Osteoclasts secrete acid and proteases that
Ca ++ Ca ++ result in dissolution of the mineralized matrix of bone
ECF Ca ++ and mobilize calcium and phosphorus.
Extracellular iCa concentration is the actively
regulated fraction of total calcium (tCa). 81,115 When
blood iCa concentration decreases, PTH secretion is
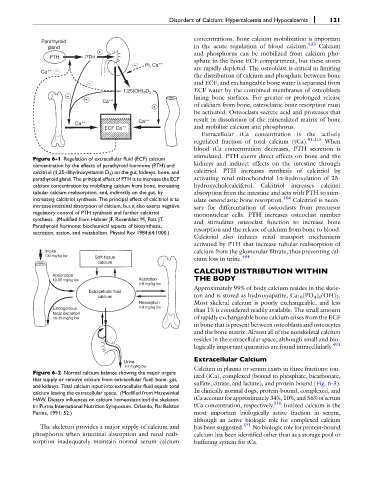
Figure 6-1 Regulation of extracellular fluid (ECF) calcium stimulated. PTH exerts direct effects on bone and the
concentration by the effects of parathyroid hormone (PTH) and kidneys and indirect effects on the intestine through
calcitriol (1,25-dihydroxyvitamin D 3 ) on the gut, kidneys, bone, and calcitriol. PTH increases synthesis of calcitriol by
parathyroid gland. The principal effect of PTH is to increase the ECF activating renal mitochondrial 1a-hydroxylation of 25-
calcium concentration by mobilizing calcium from bone, increasing hydroxycholecalciferol. Calcitriol increases calcium
tubular calcium reabsorption, and, indirectly on the gut, by absorption from the intestine and acts with PTH to stim-
increasing calcitriol synthesis. The principal effect of calcitriol is to ulate osteoclastic bone resorption. 104 Calcitriol is neces-
increase intestinal absorption of calcium, but it also exerts negative sary for differentiation of osteoclasts from precursor
regulatory control of PTH synthesis and further calcitriol mononuclear cells. PTH increases osteoclast number
synthesis. (Modified from Habner JF, Rosenblatt M, Pott JT.
Parathyroid hormone: biochemical aspects of biosynthesis, and stimulates osteoclast function to increase bone
secretion, action, and metabolism. Physiol Rev 1984;64:1000.) resorption and the release of calcium from bone to blood.
Calcitriol also induces renal transport mechanisms
activated by PTH that increase tubular reabsorption of
Intake calcium from the glomerular filtrate, thus preventing cal-
100 mg/kg bw 404
Soft-tissue cium loss in urine.
calcium
CALCIUM DISTRIBUTION WITHIN
Absorption
10-35 mg/kg bw Accretion THE BODY
4-8 mg/kg bw
Approximately 99% of body calcium resides in the skele-
Extracellular fluid
calcium ton and is stored as hydroxyapatite, Ca 10 (PO 4 ) 6 (OH) 2 .
Resorption Most skeletal calcium is poorly exchangeable, and less
Endogenous 4-8 mg/kg bw than 1% is considered readily available. The small amount
fecal excretion
10-30 mg/kg bw of rapidly exchangeable bone calcium arises from the ECF
in bone that is present between osteoblasts and osteocytes
and the bone matrix. Almost all of the nonskeletal calcium
resides in the extracellular space, although small and bio-
491
logically important quantities are found intracellularly.
Extracellular Calcium
Urine
1-7 mg/kg bw Calcium in plasma or serum exists in three fractions: ion-
Figure 6-2 Normal calcium balance showing the major organs
that supply or remove calcium from extracellular fluid: bone, gut, ized (iCa), complexed (bound to phosphate, bicarbonate,
and kidneys. Total calcium input into extracellular fluid equals total sulfate, citrate, and lactate), and protein bound (Fig. 6-3).
calcium leaving the extracellular space. (Modified from Hazewinkel In clinically normal dogs, protein-bound, complexed, and
HAW. Dietary influences on calcium homeostasis and the skeleton. iCa account for approximately 34%, 10%, and 56% of serum
In: Purina International Nutrition Symposium. Orlando, Fla: Ralston tCa concentration, respectively. 516 Ionized calcium is the
Purina, 1991: 52.) most important biologically active fraction in serum,
although an active biologic role for complexed calcium
The skeleton provides a major supply of calcium and has been suggested. 571 No biologic role for protein-bound
phosphorus when intestinal absorption and renal reab- calcium has been identified other than as a storage pool or
sorption inadequately maintain normal serum calcium buffering system for iCa.