Page 136 - Fluid, Electrolyte, and Acid-Base Disorders in Small Animal Practice
P. 136
126 ELECTROLYTE DISORDERS
Carboxyl
PTH
fragments
Circulation
H N 1 84 COOH H N 1 ? 84 COOH
2
2
Intact PTH Carboxyl fragments
GFR + Tubular
metabolism
GFR
only
Hepatic
metabolism
Renal
clearance
Bone
metabolism Urine: 1. Intact PTH - from Filtration
2. Carboxyl fragments - from Filtration
+ Tubular degradation of intact PTH
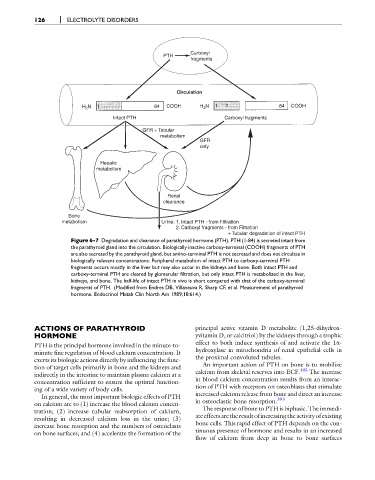
Figure 6-7 Degradation and clearance of parathyroid hormone (PTH). PTH (1-84) is secreted intact from
the parathyroid gland into the circulation. Biologically inactive carboxy-terminal (COOH) fragments of PTH
are also secreted by the parathyroid gland, but amino-terminal PTH is not secreted and does not circulate in
biologically relevant concentrations. Peripheral metabolism of intact PTH to carboxy-terminal PTH
fragments occurs mostly in the liver but may also occur in the kidneys and bone. Both intact PTH and
carboxy-terminal PTH are cleared by glomerular filtration, but only intact PTH is metabolized in the liver,
kidneys, and bone. The half-life of intact PTH in vivo is short compared with that of the carboxy-terminal
fragments of PTH. (Modified from Endres DB, Villaneuva R, Sharp CF, et al. Measurement of parathyroid
hormone. Endocrinol Metab Clin North Am 1989;18:614.)
ACTIONS OF PARATHYROID principal active vitamin D metabolite (1,25-dihydrox-
HORMONE yvitamin D, or calcitriol) by the kidneys through a trophic
effect to both induce synthesis of and activate the 1a-
PTH is the principal hormone involved in the minute-to-
hydroxylase in mitochondria of renal epithelial cells in
minute fine regulation of blood calcium concentration. It
the proximal convoluted tubules.
exerts its biologic actions directly by influencing the func-
An important action of PTH on bone is to mobilize
tion of target cells primarily in bone and the kidneys and 102
calcium from skeletal reserves into ECF. The increase
indirectly in the intestine to maintain plasma calcium at a
in blood calcium concentration results from an interac-
concentration sufficient to ensure the optimal function-
tion of PTH with receptors on osteoblasts that stimulate
ing of a wide variety of body cells.
increased calcium release from bone and direct an increase
In general, the most important biologic effects of PTH 393
in osteoclastic bone resorption.
on calcium are to (1) increase the blood calcium concen-
tration; (2) increase tubular reabsorption of calcium, The response of bone to PTH is biphasic. The immedi-
resulting in decreased calcium loss in the urine; (3) ateeffectsaretheresult ofincreasingthe activity ofexisting
increase bone resorption and the numbers of osteoclasts bone cells. This rapid effect of PTH depends on the con-
tinuous presence of hormone and results in an increased
on bone surfaces; and (4) accelerate the formation of the
flow of calcium from deep in bone to bone surfaces